The incidence of chronic myeloid leukemia (CML) in the United States has been reported to be 1.75/100,000. Older age and male patients are more likely to be diagnosed with CML (Chen Y et al. Trends in chronic myeloid leukemia incidence and survival in the United States from 1975 to 2009. Leuk Lymphoma. 2013 Jul;54(7):1411-7). Since their introduction in 2000, the mainstay of treatment for CML has been tyrosine kinase inhibitors (TKIs). These medications are generally well-tolerated. Of the TKIs in use today, Ponatinib is known to have adverse vascular events but is not recommended for use in the first line. Nilotinib has also been shown to have adverse arterial events, which tend to occur late in the treatment course (Rea D. Management of adverse events associated with tyrosine kinase inhibitors in chronic myeloid leukemia. Ann Hematol. 2015 Apr;94 Suppl 2:S149-58.). In this study, we evaluated the thrombosis and bleeding complications of CML in the era of TKIs.
The Sergeant First Class (SFC) Heath Robinson Honoring our Promise to Address Comprehensive Toxics (PACT) Act is a law that expanded Veterans' health care and benefits to those with exposure to carcinogens such as Agent Orange (AO). The PACT Act has a list of presumptive conditions due to exposure to AO. Myeloid malignancies have not been added to the presumptive list due to insufficient evidence from the Veterans and Agent Orange: Update 11 (2018). We also investigated the association of CML and AO exposure.
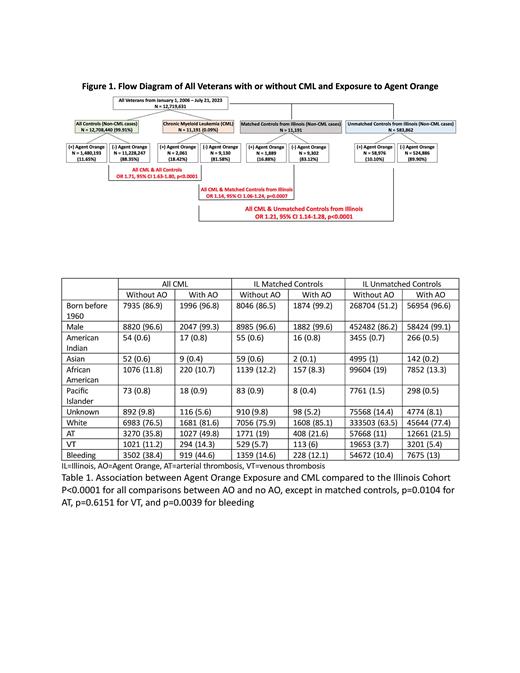
We performed a case control study from January 1, 2006 - January 26, 2023, by utilizing the Veterans Affairs Informatics and Computing Infrastructure (VINCI) database to characterize the association of AO exposure with development of CML. ICD-9 and -10 codes identified Veterans with CML, arterial thrombosis (AT), venous thrombosis (VT), and bleeding. Age-, sex-, and race-matched controls (1:1) were selected from VINCI, who are Veterans without CML from Illinois, the state most representative of the U.S. population. Exposure to Agent Orange was self-reported and verified through Veterans' duration and location of service. We stratified the Veterans according to birth year (born before or after 1960) as those born before 1960 are most likely to have AO exposure. Qualitative data were compared by chi-square tests.
When comparing all Veterans with CML and Veterans without CML, AO exposure is associated with the development of CML, OR 1.71, 95% CI 1.63-1.80, p<0.0001 (Figure 1). When adjusting for birth year and comparing all Veterans with CML unmatched controls from Illinois, there remains a statistically significant association, OR 1.21, 95% CI 1.14-1.28, p<0.0001. Further comparison to a group of matched controls is also statistically significant, OR 1.14, 95% CI 1.06-1.24, p=0.0007. Veterans born before 1960 and Males were significantly associated with development of CML, OR 6.25 95% CI 5.89-6.63 and OR 4.79 95% CI 4.29-5.36, both p<0.0001. Table 1 details the demographics and clinical characteristics among Veterans with or without CML, with or without AO exposure, and matched and unmatched controls.
When comparing all Veterans with CML and matched controls, we observed an association of CML with bleeding (OR 3.95, 95% CI 3.70-4.22), AT (OR 2.58, 95% CI 2.43-2.74), and VT (OR 2.19, 95% CI 1.98-2.41), all p<0.0001. We then investigated whether AO exposure increases the risk of AT, VT, and among Veterans with CML. When adjusting for birth year, we observed an increased risk of AT (OR 1.35, 95% CI 1.21-1.51, p<0.0001) and bleeding (OR 1.13, 95% CI 1.02-1.26, p=0.02) among Veterans with CML with AO exposure but not VT (OR 1.17, 95% CI 0.99-1.37, p=0.05).
Our analysis demonstrates a positive association between previous exposure to AO and subsequent development of CML in Veterans. These findings suggest that CML is the second myeloid malignancy to be associated with AO exposure apart from myeloproliferative neoplasms (J Clin Oncology 2023 41:16_suppl, 7011). We also demonstrate a strong association in patients with CML and outcomes including AT, VT, and bleeding. This is the first large cohort study to demonstrate these associations. These outcomes may be affected by tyrosine kinase inhibitors for the treatment of CML. Further investigation will include overall survival data, specific prognostic factors related to CML, cardiovascular risk factors, and information on the timing of AT, VT, and bleeding in relation to disease diagnosis and treatment onset.
Disclosures
Kessler:Novo Nordisk: Other: Scientific advisory board; Genentech: Other: Scientific advisory board; CSL Behring: Other: Scientific advisory board; Octapharma: Other: Scientific advisory board, Research Funding; Bayer: Consultancy, Other: Chair, DSMB, scientific advisory board, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal